Cardiac Patients Affected by Shutdowns, Predisposition to Virus; COVID-19 Patients Develop Cardiac Comorbidities
There were no protocols for courses of care, no established therapeutics, no best practices at all for this entirely new virus. “You bet it was different than anything I’ve had to deal with before. This country hasn’t experienced anything like this since 1918,” said Samuel Suede, MD, FACC, the chief of cardiology at Englewood Health and a cardiologist at Cardiovascular Associates of North Jersey, part of the Englewood Health Physician Network.
Even in the event of an extremely virulent flu strain, providers would have a robust body of literature on which to rely. With COVID-19, at the very beginning, it was one part mystery and another part speed. “This thing came on really, really fast,” said Dr. Suede, also the medical director of the Department of Cardiac Rehabilitation and the nuclear cardiology laboratory at Englewood Health. “We didn’t necessarily know how to treat people. We didn’t necessarily know how to triage people. We weren’t sure what precautions were necessary and what weren’t.”
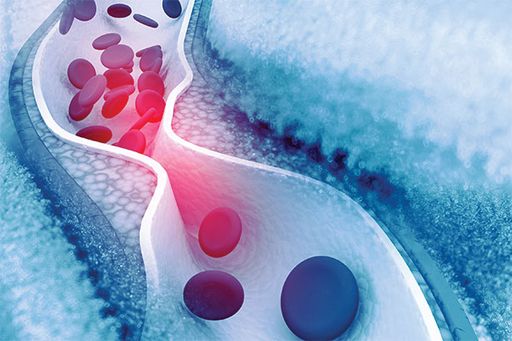
COVID-19 entered the public’s awareness and the medical canon as a disease of the airways. “We thought this was another respiratory virus,” Dr. Suede said. It was also clear from the beginning that there were apparent high-risk populations: the elderly and those with preexisting conditions, such as hypertension, diabetes or cardiac ailments. “We’ve since learned,” Dr. Suede said, “there are a lot of cardiac complications of COVID such as myocarditis, pericarditis, acute myocardial infarction, arrhythmias, pulmonary emboli and thromboembolic events” (JAMA Cardiol 2020;5[7]:811-818; Circulation 2020;141[20]:1648-1655).
A Responsive Health Care System
Englewood Health reacted quickly at the onset of the pandemic. “As we started learning in March about the severity of COVID, we stopped doing all elective procedures to keep the beds available for the COVID patients,” said Mahesh Bikkina, MD, an interventional cardiologist with HVA Medical Group, part of the Englewood Health Physician Network.
To keep the patients safe, “the hospital transitioned very quickly and very early to telemedicine,” said Aron Schwarcz, MD, an interventional cardiologist also with Cardiovascular Associates of North Jersey. “Very few procedures were being performed. The stress lab’s work was closed. Only select inpatients were getting echos.”
As the patient–doctor relationships shifted online, so did the doctor–doctor consults. “The cardiology section has a conference every Wednesday morning, about 40 people, 50 people in a conference room. We decided to continue that conference by Zoom,” Dr. Suede said. “One, attendance has never been better. But secondly, it was an opportunity for us to communicate. So, everyone was very much abreast of what was happening and into our cardiology patients and how we were modifying treatment plans for the COVID population.”
As doctors conferred with one another and with colleagues around the world, the cardiac complications of COVID-19 came into focus. Englewood Health’s administration went to work again, this time creating a COVID-19 cardiac floor. “Any patients who had COVID, who had any either previous cardiac condition or were having some cardiac complications, but did not require an ICU setting, went to that floor,” Dr. Schwarcz said. “Fifty beds, taken care of by cardiologists,” Dr. Bikkina said, “because we can do the best job for those patients.”
The trust in the administration, the faith that providers have in the systems and support, the ability of the whole organization—topdown—to adapt was at the heart of Englewood Health’s response. “I feel very lucky to have worked at Englewood during this pandemic because I think the administration and the medical staff were very responsive, very resourceful, very quick-footed, and instituted a lot of changes and protocols so we can treat this huge influx of very sick patients,” Dr. Suede said.
Cardiac Prophylaxis
Very early in the pandemic, it became clear that “there are two main effects that we see in patients with COVID,” said Dr. Bikkina, who is also an associate professor of medicine at New York Medical College, in Valhalla, N.Y. “One, the virus affecting the heart muscle and the muscle gets weaker; the second, blood clots are forming at a much higher rate in COVID patients.” Englewood Health’s administration and providers alike put their individual competence and readiness to the test.
The COVID–Cardiac floor that the administration implemented at the outset “provided another level of care for all these cardiac patients who may have gone unrecognized, or maybe their cardiac issues may have sort of taken a little bit of a back seat because of COVID,” Dr. Schwarcz said. But it had another, maybe unexpected benefit: the added attention from cardiac specialists.
It wasn’t long before “we realized that there was a high percentage of patients who were having thromboembolic complications. So we started measuring d-dimer levels to determine who needed prophylactic anticoagulation,” Dr. Schwarcz said. With the full support of the administration, “protocols were established by the COVID team and we prophylactically anticoagulated to prevent thromboembolic complications. That really put cardiologists at the front line of this.”
Cause for Optimism
As this article was written, case and mortality rates rose across the United States and the world and may remain high for a period. A potentially underrecognized casualty from early in the pandemic is people “who should have gotten care, but did not get the care that they needed because they were too scared to go to the hospitals, too worried to go to the offices,” Dr. Schwarcz said. Dr. Bikkina highlighted the danger caused by that hesitation. “Even though they’re having chest pain, they do not want to go to the hospital because they’re afraid of COVID, and then they end up having heart attacksand strokes and dying at home.”
In the months ahead, there is cause for optimism. “The treatment that we have now, with [the COVID] testing that we have now, we’ll be able to keep up elective [procedures],” Dr. Schwarcz said. Patients will not have to put off improving their quality of life. Englewood Health will continue to work collaboratively, as evinced by the administration’s pragmatic leadership, working hand-in-hand with the accountability, adaptability and inventiveness of the providers.
“We want to let the public know,” Dr. Bikkina said, “when a new patient comes, it is very safe for them to get the care that is needed for them.”
Posted August 16, 2021