Compared with classic open procedures or laparoscopy, robotic-assisted colorectal surgery allows for minimally invasive, highly accurate procedures, which have been shown to have higher functional outcomes, according to a meta-analysis published last year in Surgical Endoscopy (2021;35[1]:81-95).
In the combined analysis of more than 24,000 patients, individuals who received robotic-assisted rectal resection were found to have a lower rate of urinary retention and ileus and higher quality of life when compared with
laparoscopic surgery.
“Robotic-assisted surgery provides the highest level of dexterity and a nearly three-dimensional view so we can better see the patient’s anatomy,” said Peter M. Kaye, MD, a colon and rectal surgeon at Englewood Health. “The surgery is less invasive, there is less pain and there is less time spent in the hospital.”
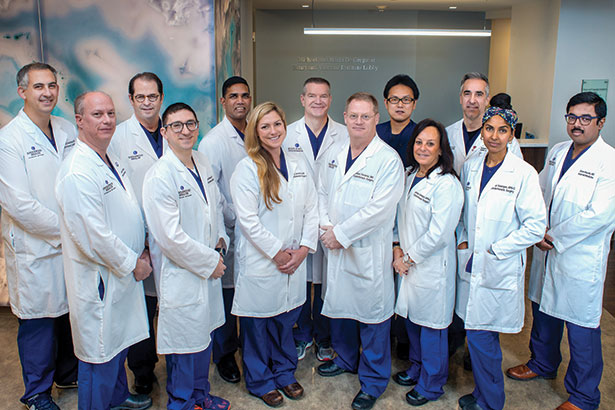
A dedication to the skilled use of emerging surgical technologies, as well as a strong multidisciplinary team approach, has allowed Englewood Health to offer cutting-edge therapies for patients with colorectal and digestive cancers.
The team at Englewood Health has completed more than 1,000 robotic resections for cancer. “We are the most experienced robotic colorectal surgeons in the area,” Dr. Kaye said. “This is what we’re trained to do.”
One important benefit of the robotic approach is the decreased rate of conversion to an open procedure, which in turn reduces postoperative complication rates and allows for a faster interval to completing chemotherapy (Ann Laparosc Endosc Surg 2020;5:9). Being able to perform complex surgeries in a minimally invasive way also benefits patients by decreasing the need for devices, such as colostomy bags.
“Very few surgeons have the technical ability to conduct sphincter-sparing surgery,” said Anna Serur, MD, the chief of colon and rectal surgery at Englewood Health (J Gastrointestinal Surg 2014;18[7]:1358-1372). “Fortunately, we have the special expertise to do these challenging procedures.”
Drs. Serur and Kaye also emphasized the importance of Englewood Health’s strong, multidisciplinary approach to managing patients’ cancers.
“We work very closely with a patient’s medical oncologist, radiation oncologist, with all of the specialties involved in the patient’s care,” Dr. Kaye commented.
Dr. Serur agreed that the team approach in the cancer center is part of what makes Englewood Health stand out. “We take pride in providing excellent care and outcomes,” she said. “We use the latest techniques and medicines, and follow best practices and national recommendations as they are released. We provide our patients with an experience that is special.”
Posted August 20, 2021
Advances in Cardiologic Assessment For Oncology Patients
While cardiac toxicity from chemotherapy treatments is a known challenge in oncology, previous imaging techniques have sometimes missed spotting affected patients. Now, a novel imaging technology, speckle tracking echocardiography, allows for earlier and more accurate monitoring of heart function in a variety of oncology patients (Tex Heart Inst J 2020;47[2]:96-107).
“Although cardiology assessment of oncology patients is a rather new specialty, the effect of certain chemotherapy drugs on the heart has been known for many years,” said Jay A. Erlebacher, MD, a cardiologist in the Englewood Health Physician Network. “However, as some of these treatments have become the backbone of treatment for many diseases, particularly breast cancer, it is increasingly important to detect the toxicities of oncology drugs, which are potentially toxic to the heart.”
Dr. Erlebacher said it is crucial that these toxicities be detected as early as possible so adverse consequences on the heart can be avoided.
The headline drug for treating many cancers is doxorubicin, which is frequently used in breast cancer, but has potential toxicity related to the cumulative dose of the drug, according to Dr. Erlebacher. This can weaken the heart, potentially leading to congestive heart failure (CHF), he added.
Echocardiography is used routinely to monitor heart and valvular function in patients with heart disease or suspected heart disease. “We primarily look at a performance measurement of the heart called ejection fraction [EF], similar to measuring the horsepower of the heart,” said Dr. Erlebacher, who led Englewood Health’s echocardiography lab for the past 25 years. EF measures the percentage of blood that is ejected from the heart with each beat, typically measured between 55% and 70%. An EF that falls by 10 percentage points and drops below 53% has been used as a definition of chemotherapy-induced cardiac toxicity. Advanced echocardiogram machines are now able to recreate the left ventricular pumping chamber in 3D to obtain a more accurate and reproducible EF measurement than older more traditional techniques. Understanding a patient’s EF is an important step in diagnosing and treating disease.
Doxorubicin and the other major cancer drug potentially toxic to the heart, trastuzumab, can lower EF and impair the performance of the heart, which can result in excess fluid in the body. “The legs become waterlogged and swollen, and patients will suffer shortness of breath, the hallmarks of CHF,” Dr. Erlebacher said.
Fortunately, subtle effects that these two drugs can have on the heart may now be detected even before EF begins to decrease.
Speckle tracking echocardiography is a relatively new technology that is more sensitive and capable of measuring heart dysfunction earlier. “Within the heart muscle, there are tiny dots called speckles,” Dr. Erlebacher said. “Extremely advanced processing software actually tracks the motion of each individual speckle within the view of the heart and computes the relative motion of adjacent speckles.”
By measuring these speckles in relative motion as the heart contracts, a measurement of the regional and global function of the heart can be derived via global longitudinal strain (GLS).
“In many ways, GLS is a superior measurement of heart function compared to EF,” Dr. Erlebacher said. “GLS tends to be more reproducible and tends to start going south and becomes worse even before EF is affected. GLS is an ideal way of tracking patients who receive these chemotherapy drugs.”
Patients are monitored both before and during chemotherapy with 3D echocardiography and speckle tracking. Trastuzumab patients are followed every three months, whereas doxorubicin patients are assessed upon completion of drug therapy or when they reach a standardized dose. Doxorubicin patients are tested again six months after completing a course of treatment.
“If the heart function is decreasing, there are a number of treatments that have been shown to improve left ventricular function, similar to therapies for any type of CHF due to reduced heart function, including betablockers and angiotensin-converting enzyme inhibitors,” Dr. Erlebacher said. “But for Herceptin [trastuzumab], simply temporarily withdrawing the drug will usually cause the heart to improve on its own over time. Our goal in working with our oncology colleagues is for our patients to receive their lifesaving chemotherapy without compromising their heart function.”
Posted August 17, 2021
COVID-19 Hits Cardiac Care In Multiple Ways
Cardiac Patients Affected by Shutdowns, Predisposition to Virus; COVID-19 Patients Develop Cardiac Comorbidities
There were no protocols for courses of care, no established therapeutics, no best practices at all for this entirely new virus. “You bet it was different than anything I’ve had to deal with before. This country hasn’t experienced anything like this since 1918,” said Samuel Suede, MD, FACC, the chief of cardiology at Englewood Health and a cardiologist at Cardiovascular Associates of North Jersey, part of the Englewood Health Physician Network.
Even in the event of an extremely virulent flu strain, providers would have a robust body of literature on which to rely. With COVID-19, at the very beginning, it was one part mystery and another part speed. “This thing came on really, really fast,” said Dr. Suede, also the medical director of the Department of Cardiac Rehabilitation and the nuclear cardiology laboratory at Englewood Health. “We didn’t necessarily know how to treat people. We didn’t necessarily know how to triage people. We weren’t sure what precautions were necessary and what weren’t.”
COVID-19 entered the public’s awareness and the medical canon as a disease of the airways. “We thought this was another respiratory virus,” Dr. Suede said. It was also clear from the beginning that there were apparent high-risk populations: the elderly and those with preexisting conditions, such as hypertension, diabetes or cardiac ailments. “We’ve since learned,” Dr. Suede said, “there are a lot of cardiac complications of COVID such as myocarditis, pericarditis, acute myocardial infarction, arrhythmias, pulmonary emboli and thromboembolic events” (JAMA Cardiol 2020;5[7]:811-818; Circulation 2020;141[20]:1648-1655).
A Responsive Health Care System
Englewood Health reacted quickly at the onset of the pandemic. “As we started learning in March about the severity of COVID, we stopped doing all elective procedures to keep the beds available for the COVID patients,” said Mahesh Bikkina, MD, an interventional cardiologist with HVA Medical Group, part of the Englewood Health Physician Network.
To keep the patients safe, “the hospital transitioned very quickly and very early to telemedicine,” said Aron Schwarcz, MD, an interventional cardiologist also with Cardiovascular Associates of North Jersey. “Very few procedures were being performed. The stress lab’s work was closed. Only select inpatients were getting echos.”
As the patient–doctor relationships shifted online, so did the doctor–doctor consults. “The cardiology section has a conference every Wednesday morning, about 40 people, 50 people in a conference room. We decided to continue that conference by Zoom,” Dr. Suede said. “One, attendance has never been better. But secondly, it was an opportunity for us to communicate. So, everyone was very much abreast of what was happening and into our cardiology patients and how we were modifying treatment plans for the COVID population.”
As doctors conferred with one another and with colleagues around the world, the cardiac complications of COVID-19 came into focus. Englewood Health’s administration went to work again, this time creating a COVID-19 cardiac floor. “Any patients who had COVID, who had any either previous cardiac condition or were having some cardiac complications, but did not require an ICU setting, went to that floor,” Dr. Schwarcz said. “Fifty beds, taken care of by cardiologists,” Dr. Bikkina said, “because we can do the best job for those patients.”
The trust in the administration, the faith that providers have in the systems and support, the ability of the whole organization—topdown—to adapt was at the heart of Englewood Health’s response. “I feel very lucky to have worked at Englewood during this pandemic because I think the administration and the medical staff were very responsive, very resourceful, very quick-footed, and instituted a lot of changes and protocols so we can treat this huge influx of very sick patients,” Dr. Suede said.
Cardiac Prophylaxis
Very early in the pandemic, it became clear that “there are two main effects that we see in patients with COVID,” said Dr. Bikkina, who is also an associate professor of medicine at New York Medical College, in Valhalla, N.Y. “One, the virus affecting the heart muscle and the muscle gets weaker; the second, blood clots are forming at a much higher rate in COVID patients.” Englewood Health’s administration and providers alike put their individual competence and readiness to the test.
The COVID–Cardiac floor that the administration implemented at the outset “provided another level of care for all these cardiac patients who may have gone unrecognized, or maybe their cardiac issues may have sort of taken a little bit of a back seat because of COVID,” Dr. Schwarcz said. But it had another, maybe unexpected benefit: the added attention from cardiac specialists.
It wasn’t long before “we realized that there was a high percentage of patients who were having thromboembolic complications. So we started measuring d-dimer levels to determine who needed prophylactic anticoagulation,” Dr. Schwarcz said. With the full support of the administration, “protocols were established by the COVID team and we prophylactically anticoagulated to prevent thromboembolic complications. That really put cardiologists at the front line of this.”
Cause for Optimism
As this article was written, case and mortality rates rose across the United States and the world and may remain high for a period. A potentially underrecognized casualty from early in the pandemic is people “who should have gotten care, but did not get the care that they needed because they were too scared to go to the hospitals, too worried to go to the offices,” Dr. Schwarcz said. Dr. Bikkina highlighted the danger caused by that hesitation. “Even though they’re having chest pain, they do not want to go to the hospital because they’re afraid of COVID, and then they end up having heart attacksand strokes and dying at home.”
In the months ahead, there is cause for optimism. “The treatment that we have now, with [the COVID] testing that we have now, we’ll be able to keep up elective [procedures],” Dr. Schwarcz said. Patients will not have to put off improving their quality of life. Englewood Health will continue to work collaboratively, as evinced by the administration’s pragmatic leadership, working hand-in-hand with the accountability, adaptability and inventiveness of the providers.
“We want to let the public know,” Dr. Bikkina said, “when a new patient comes, it is very safe for them to get the care that is needed for them.”
Posted August 16, 2021
Cancer Survivor Day
Today, there are 14 million cancer survivors living in the United States. As National Cancer Survivors Month comes to a close, our Englewood Health providers and team members at The Lefcourt Family Cancer Treatment and Wellness Center have put together a special video to celebrate survivors and offer practical advice to help you throughout your survivorship journey.
Posted July 1, 2021
It Only Gets Better – With BergenPAC

Englewood Health and BergenPAC have teamed up to bring you this special performance and message.
Vaccines work. Stay safe. Stay healthy.
Posted June 24, 2021
Englewood Health Performs 1000th Transcatheter Aortic Valve Replacement
June 14, 2021 — The heart valve team at Englewood Hospital successfully performed its 1000th transcatheter aortic valve replacement (TAVR) procedure on a patient suffering from aortic stenosis, a debilitating type of heart disease. Initially one of the first hospitals in New Jersey to offer the procedure following its approval by the FDA in 2011, Englewood has become one of the leading TAVR centers in New Jersey.
The TAVR procedure was originally offered as an alternative treatment for patients with aortic stenosis who were not candidates for open-heart surgery due to their age or risk for complications. Since then, it has expanded to lower risk patients. Aortic stenosis, a narrowing of the valve, often leads to symptoms such as shortness of breath, lightheadedness, and fatigue.
“I’m so proud to work with such an accomplished team,” said Dr. Ramin Hastings, medical director of the structural heart and valve program. “Through the support of our community we have created a program that provides local expertise with outcomes in the top 10% of the country. Having cared for 1000 TAVR patients is a remarkable milestone for Englewood Health.”
Eliminating the need for open-heart surgery, the TAVR procedure allows an artificial valve to be implanted through a catheter that is inserted in the artery of the patient’s leg or chest. The TAVR team at Englewood Hospital, consisting of both interventional cardiologists and cardiothoracic surgeons who work together to perform the procedure, has observed a high success rate in TAVR patients, with outcomes better than the national average.
“It is an honor to celebrate this achievement with our entire team,” says Denise Goldstein, structural heart and valve program coordinator at Englewood Hospital. “Through the dedication and expertise of our multidisciplinary team, we have performed 1000 cases, with great results. We are extremely proud of this huge accomplishment.”
The treatment offers patients a less-invasive option with a quicker recovery, generally allowing them to return home the next day.
To learn more about the procedure and the Structural Heart and Valve Program, visit www.englewoodhealth.org/heart.
American Heart Association Honors Englewood Health at New Jersey Heart Ball
Dr. Samuel Suede, chief of cardiology, named Physician of the Year in Cardiology
June 4, 2021 — Dr. Samuel Suede, chief of cardiology at Englewood Health, received the Physician of the Year in Cardiology award from the American Heart Association, the world’s leading nonprofit organization focused on heart and brain health for all, at its virtual New Jersey Heart Ball last evening. This annual event is a celebration of life and serves to raise awareness of heart disease and stroke, while also highlighting clinical excellence and advancements in these areas across New Jersey.
“Dr. Suede is what I like to call a comprehensive cardiologist,” said Warren Geller, president and CEO of Englewood Health. “He is an outstanding communicator who looks at the whole patient, including their environment and family history. The American Heart Association could not have selected a better physician, or ambassador, to honor and to carry this message forward.”
Dr. Suede was recognized for his leadership, collaboration with physicians across multiple specialties, dedication to improving patient outcomes, and the positive influence he has had on his patients and the medical community of northern New Jersey.
Englewood Hospital Achieves Healthgrades 2021 Patient Safety Excellence Award™
Hospital ranks in top 10% in the nation for patient safety
May 12, 2021 — Englewood Hospital has received the 2021 Patient Safety Excellence Award™ from Healthgrades, placing it among the top 10% of hospitals in the nation for patient safety.
“Receiving the Patient Safety Excellence Award from Healthgrades speaks to our commitment of ensuring that each of our patients receives the safest, most personalized medical care,” said Kathleen Kaminsky, MS, RN, NE-BC, senior vice president of patient care services and chief nursing officer at Englewood Health. “As operations transition to a new normal in hospitals across the country, our patients and visitors can be assured that we are taking every step to ensure their safety.”
From 2017 through 2019, there were 190,273 potentially preventable patient safety events among Medicare patients reported in U.S. hospitals.* Healthgrades found that patients treated in hospitals receiving the Healthgrades 2021 Patient Safety Excellence Award were, on average*:
- 50.3% less likely to experience a collapsed lung due to a procedure or surgery in or around the chest than patients treated at non-recipient hospitals.*
- 60.3% less likely to experience an in-hospital fall resulting in hip fracture than patients treated at non-recipient hospitals.*
- 66.5% less likely to experience pressure sores or bed sores acquired in the hospital than patients treated at non-recipient hospitals.*
- 65.4% less likely to experience catheter-related bloodstream infections acquired in the hospital than patients treated at non-recipient hospitals.*
If all hospitals, as a group, performed similarly to those performing better than expected on each of the 13 Patient Safety Indicators (PSIs) evaluated by Healthgrades, on average, 106,052 patient safety events could have been avoided.*
“The importance of hospital quality is now at the forefront of consumers’ minds, especially as we continue to navigate COVID-19. We congratulate the recipients of the Healthgrades 2021 Patient Safety Excellence Award for their ongoing commitment to upholding the highest quality standards for their patients and communities,” said Brad Bowman, MD, chief medical officer for Healthgrades.
See the full Healthgrades 2021 hospital ratings and quality methodologies.
*Statistics are calculated from Healthgrades Patient Safety Ratings and Excellence Award methodology, which is based primarily on AHRQ technical specifications (Version 2020.0.1) to MedPAR data for years 2017 through 2019, and represent three-year estimates for Medicare patients only.
Englewood Hospital Nationally Recognized with ‘A’ for Spring 2021 Leapfrog Hospital Safety Grade
April 29, 2021 — Englewood Hospital was awarded an “A” grade in hospital safety today, as The Leapfrog Group released its Spring 2021 safety grades. This national distinction recognizes the hospital’s achievements in providing safe health care. The Leapfrog Group is an independent national watchdog organization dedicated to health care quality and safety.
“We are proud to receive this national recognition from The Leapfrog Group,” said Kathleen Kaminsky, MS, RN, NE-BC, senior vice president of patient care services and chief nursing officer at Englewood Health. “The primary goal at Englewood Hospital is to provide each patient with an exceptional experience. This is accomplished through the commitment of our entire healthcare team to hold ourselves to the highest standards of both quality and safety.”
Developed under the guidance of a national Expert Panel, the Leapfrog Hospital Safety Grade uses up to 27 measures of publicly available hospital safety data to assign grades to more than 2,700 U.S. acute-care hospitals twice per year.
“An ‘A’ safety grade is an elite designation that your community should be proud of,” said Leah Binder, president and CEO of The Leapfrog Group. “The past year has been extraordinarily difficult for hospitals, but Englewood Hospital shows us it is possible to keep a laser focus on patients and their safety, no matter what it takes.”
The Hospital Safety Grade’s methodology is peer reviewed, and the results are available to the public. To see Englewood Health’s full grade details and access patient tips for staying safe in the hospital, visit hospitalsafetygrade.org and follow The Leapfrog Group on Twitter and Facebook.