One of the unique surgeries performed at Englewood Health that is not offered by many other health systems is bloodless spinal deformity surgery, which is reserved for patients such as Jehovah’s Witnesses, for whom blood transfusion is not an option. “Spinal deformity surgery is associated with significant blood loss, often requiring the transfusion of blood and/or blood products,” said Yakov Gologorsky, MD, a neurosurgeon at Englewood Health. Spinal deformity surgery is associated with unacceptably high rates of morbidity and mortality in patients who refuse blood or blood products, according to Dr. Gologorsky, who is also an associate clinical professor of neurosurgery at the Icahn School of Medicine at Mount Sinai, in New York City. “This is why these patients have historically been denied spinal deformity surgery,” he said.
Now, these patients can be referred to the bloodless surgery program at Englewood Health. With the help of multiple clinicians, including hematologists, patients may be pretreated with erythropoietin, a hormone that stimulates red blood cell production. The clinical team also ensures that before surgery, patients have appropriate levels of iron, folate and other essential elements to optimize their blood count.
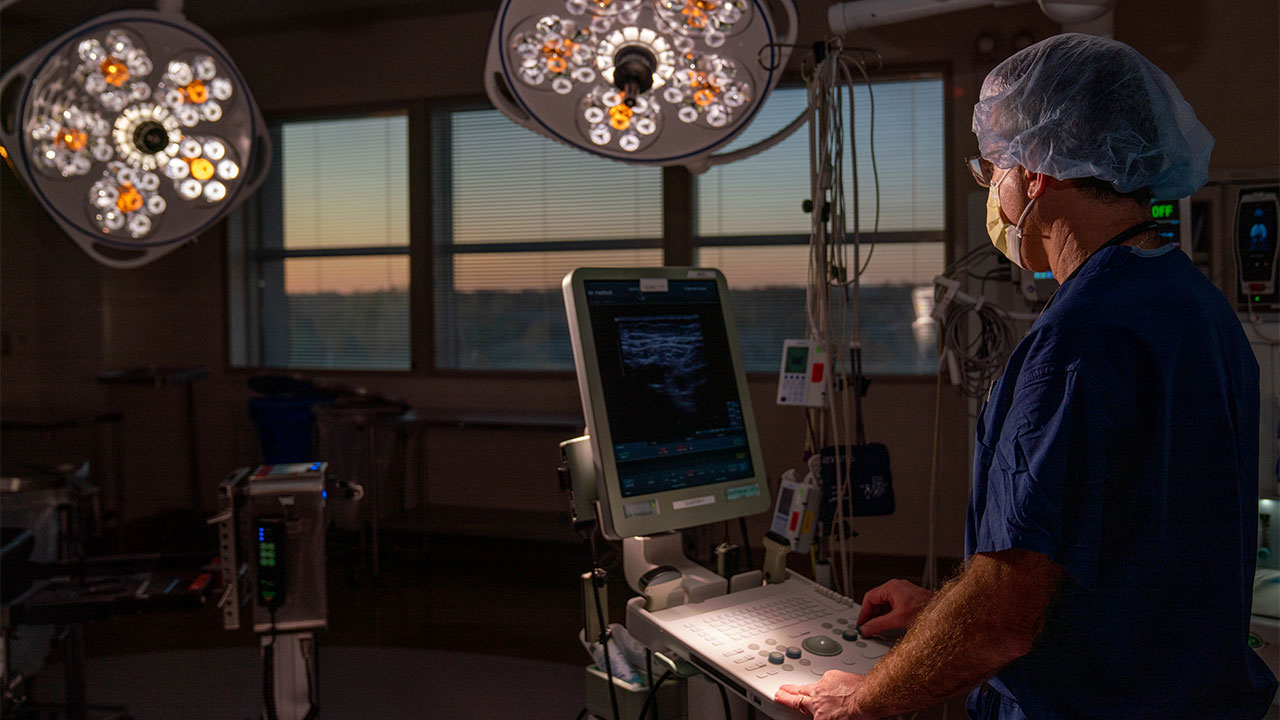
The anesthesiologist works closely with the surgeon to help minimize blood loss. Immediately prior to surgery, the anesthesiologist removes a certain volume of whole blood from the patient through acute normovolemic hemodilution and replaces it with intravenous fluids. “This process dilutes the whole blood that is present in the body,” Dr. Gologorsky said. “Hence, when a patient loses blood, they are actually losing diluted blood, which has fewer red cells.”
In the middle of surgery, the whole blood is returned to the patient to maintain the blood count within a safe range. In addition, antifibrinolytic agents such as epsilon-aminocaproic acid (Amicar) or tranexamic acid are administered perioperatively. “These agents help with clot formation and decrease blood loss,” Dr. Gologorsky said. Other blood conservation techniques that minimize the risk for transfusion, such as cell salvage, are used as well.
After surgery, which may last anywhere from two to 10 hours, patients remain hospitalized for three to 10 days. Some surgeries are purposefully staged three months apart, especially for those involving extreme deformity corrections. “In almost all instances, we are able to accomplish the goals of surgery and correct the spinal deformity,” Dr. Gologorsky said.
Dr. Gologorsky is the principal investigator of a new retrospective study of 28 patients with 34 admissions (median age, 37 years; range, 11-65 years). All patients underwent bloodless spinal deformity surgery at Englewood Health between 2002 and 2019. Of note, 50% of the cohort had significant medical comorbidities, but were still able to undergo the surgeries safely.
“Deformity correction and goals of surgery were achieved in 24 of the 28 patients,” Dr. Gologorsky said. “With proper preoperative planning and judicious use of blood conservation techniques, spinal deformity surgery may be performed safely and effectively.”
Dr. Gologorsky said the same techniques could be applied widely to the general population to minimize blood loss and the need for allogeneic blood transfusion.
“Patients are extremely pleased and truly grateful for the services that we provide,” he said. “These patients are often miserable and have undergone other surgeries. We offer them tangible results and improvement in their quality of life.”
Posted on December 18, 2020