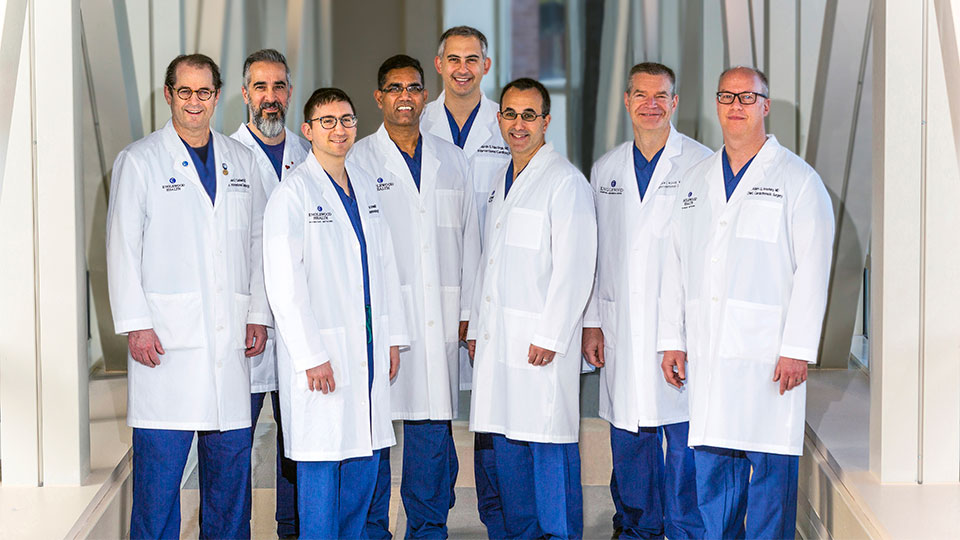
September 4, 2019 — Englewood Orthopedic Associates, a multispecialty orthopedics practice founded more than 40 years ago, has joined Englewood Health Physician Network. As the largest orthopedics practice in Bergen County, its nine orthopedic surgeons and physicians specialize in a range of clinical areas, including conditions of the hip, knee, shoulder, hand, elbow, wrist, foot, ankle, and spine; osteoporosis and metabolic bone disease; pain management; sports medicine; and trauma. New patients are welcome at its practice locations in Englewood and Paramus.
Many of Englewood Orthopedic Associates’ doctors are long-time members of Englewood Hospital’s medical staff and have held leadership positions at the hospital over the years. The specialists now joining the Englewood Health Physician Network are Adam Becker, MD; Damien Davis, MD; Jessica Fleischer, MD; Manesha Lankachandra, MD; David Nguyen, MD; Michael Pizzillo, MD; Peter Salob, MD; Richard Salzer, MD; and Asit Shah, MD, PhD.
“The Englewood Orthopedic Associates team brings expertise in all areas of surgical and non-surgical treatments of orthopedic conditions for adults, adolescents, and children to the Englewood Health Physician Network,” says Asit Shah, MD, PhD, chief of orthopedic surgery, director of the Joint Replacement Center at Englewood Hospital, and an orthopedic surgeon with Englewood Orthopedic Associates. “Whether specializing in joint replacement, pediatric or geriatric orthopedics, sports medicine, or physical medicine, each of these surgeons and physicians is dedicated to providing innovative treatment options to improve function, enhance quality of life, and allow for the quickest recovery possible for each patient.”
He adds, “By joining the Englewood Health Physician Network, our specialists will collaborate closely with primary care doctors and other specialists, through the enhanced communication and improved coordination of care enabled by the network. We now have a shared electronic medical record system and, with these advantages, we will continue to be a trusted resource for patients with bone and joint disease across northern New Jersey.”
Englewood Orthopedic Associates helps restore function in patients with musculoskeletal conditions through a full range of orthopedic services, including minimally invasive joint replacement surgery, physiatry, pain management, trauma care, and work-related injury evaluation and treatment. In addition to orthopedic surgeons, an endocrinologist, a physiatrist, and a group of orthopedic physician assistants, an on-site team of licensed physical therapists at Englewood Orthopedics provides rehabilitation services with advanced techniques and the most up-to-date equipment. Walk-in urgent care for bone, joint, and muscle injuries is available Monday through Friday, from 8:30 a.m. to 6 p.m.
“As our network continues to grow, we remain focused on ensuring that our patients have access to leading care right here, in their own backyard,” says Dr. Stephen Brunnquell, president of the Englewood Health Physician Network. “The specialists at Englewood Orthopedic Associates are leaders in their field and are skilled in the latest techniques and technologies in their subspecialties. This helps to ensure the best outcomes for our patients.”
Englewood Orthopedic Associates Physicians Joining Englewood Health Physician Network
Adam Becker, MD
Dr. Becker is board certified in orthopedic surgery. He specializes in foot and ankle care and surgery for adults and children. His primary clinical interests include leg, ankle, and foot fractures; sports injuries; ankle and foot arthritis; tendon and ligament disorders; bunions; lesser toe deformities; and complex foot and ankle reconstruction, including total ankle replacement surgery. Dr. Becker received his MD from SUNY Upstate Medical University College of Medicine. He did an orthopedic residency at the University of Medicine and Dentistry of New Jersey and a foot and ankle fellowship at Mercy Medical Center in Baltimore, Maryland. He is a member of the American Academy of Orthopaedic Surgeons and the American Orthopaedic Foot & Ankle Society. | Full profile
Damien I. Davis, MD
Dr. Davis is board certified in orthopedic surgery and holds a subspecialty certificate in Surgery of the Hand (Certificate of Added Qualification-CAQ). His primary clinical interests are disorders of the hand, wrist, elbow and shoulder. He specializes in traumatic and degenerative conditions of the upper extremity, including nerve compression disorders, and treats both pediatric and adult patients. Dr. Davis received his MD from Georgetown University School of Medicine. He did an orthopedic surgery residency at St. Luke’s-Roosevelt Hospital Center, in Manhattan, followed by a hand and upper extremity surgery fellowship at Allegheny General Hospital, in Pittsburgh. He is a member of the American Academy of Orthopaedic Surgeons and the American Society for Surgery of the Hand. | Full profile
Jessica Fleischer, MD
Dr. Fleischer is board certified in endocrinology. She specializes in osteoporosis and metabolic bone diseases and has particular expertise in the reading and interpretation of bone density tests. She has additional clinical interests in hyperparathyroidism and calcium disorders. Dr. Fleischer received her MD from SUNY Stony Brook School of Medicine. She did an internal medicine residency at the University of Pittsburgh Medical Center, where she was chief resident, followed by an endocrinology fellowship at Columbia University Medical Center. | Full profile
Manesha Lankachandra, MD
Dr. Lankachandra is board eligible in orthopedic surgery. She specializes in hand, wrist, and elbow surgery. Her clinical interests include reconstruction, trauma of the upper extremity, and nerve compression disorders. Dr. Lankachandra received her MD from the University of Kansas School of Medicine. She did an orthopedic surgery residency at the University of Missouri–Kansas City School of Medicine, followed by a shoulder and elbow fellowship at MedStar Union Memorial Hospital, in Baltimore, Maryland, and a hand fellowship at the University of California–San Francisco School of Medicine. She is a member of the American Academy of Orthopaedic Surgeons.
David Nguyen, MD
Dr. Nguyen is board certified in physical medicine and rehabilitation and in pain medicine. His primary clinical interests are musculoskeletal disorders of the spine; upper and lower extremities disorders; and complications of diabetes, joint disease, traumatic brain injury, and pain management. Dr. Nguyen received his MD from the University of California–Davis School of Medicine. He did a physical medicine and rehabilitation residency, during which he was chief resident, as well as a pain medicine fellowship, at the University of California, Los Angeles–Veterans Administration Greater Los Angeles Healthcare System. He is a member of the American Academy of Physical Medicine and Rehabilitation, the Association of Academic Physiatrists, the North American Neuromodulation Society, the North American Spine Society, and the Spine Intervention Society. | Full profile
Michael F. Pizzillo, MD
Dr. Pizzillo is board certified in orthopedic surgery and holds a subspecialty certificate (Certificate of Added Qualifications-CAQ) in both Surgery of the Hand and in Orthopedic Sports Medicine. He specializes in hand, upper extremity, and shoulder surgery. His clinical interests include arthroscopic surgery, post-traumatic reconstruction, and joint replacement of the hand and upper extremity. Dr. Pizzillo received his MD from SUNY Downstate Health Sciences University Medical College. He completed an orthopedic surgery residency at NYU Langone Medical Center, Bellevue Hospital Center, and the Manhattan VA Medical Center, followed by a hand and upper extremity fellowship at the University of Pittsburgh Medical Center. He is a fellow of the American Academy of Orthopaedic Surgeons and a member of the American Society for Surgery of the Hand and the New York Society for Surgery of the Hand. | Full profile
Peter A. Salob, MD
Dr. Salob is board certified in orthopedic surgery. His primary clinical interests are adult, adolescent, and pediatric sports medicine; knee, shoulder, hip, ankle, and foot injuries and conditions. Dr. Salob received his MD from the University of Chicago Pritzker School of Medicine. He did an orthopedic surgery residency at Montefiore Medical Center (Albert Einstein College of Medicine), in New York. He did a sports medicine fellowship, with a subspecialty in pediatric trauma and sports-related injuries, at Boston Children’s Hospital (Harvard Medical School). He is a fellow of the American Academy of Orthopedic Surgeons and a member of the American Orthopedic Society for Sports Medicine. | Full profile
Richard Louis Salzer, Jr., MD
Dr. Salzer is board certified in orthopedic surgery. He specializes in consultative orthopedic diagnosis and treatment of the adult patient. His primary clinical interests are adult hip and knee conditions and sports medicine injuries of the hip and knee. Dr. Salzer received his MD from Tufts University School of Medicine. He did a general surgery residency at Parkland Memorial Hospital and St. Paul Hospital (University of Texas), in Dallas, Texas, followed by an orthopedic surgery residency at the Hospital for Special Surgery, in Manhattan. He is a fellow of the American Academy of Orthopaedic Surgeons and a member of the American Board of Orthopedic Surgery. | Full profile
Asit K. Shah, MD, PhD
Dr. Shah is chief of orthopedic surgery, director of orthopedic implants, and a founding member of the Joint Replacement Center at Englewood Hospital. He is board certified in orthopedic surgery. His clinical interests include minimally invasive knee and hip replacement and complex revision knee and hip reconstruction. Dr. Shah received his MD, as well as a PhD in biochemistry and molecular biology, from Jefferson Medical College (now the Sidney Kimmel Medical College) of Thomas Jefferson University, in Philadelphia, where he also completed a National Institutes of Health molecular biology fellowship. He did his orthopedic surgery residency at the Mount Sinai Hospital, in Manhattan, and a hip and knee implant fellowship at Massachusetts General Hospital, in Boston. He is a fellow of the American Academy of Orthopaedic Surgeons, an oral examiner for the American Board of Orthopedic Surgery, and a member of the American Association of Hip and Knee Surgeons, and Eastern Orthopedic Association. | Full profile