Englewood Hospital Participates in Landmark Global Trial Reducing Major Infections in Cardiac Implantable Electronic Device Procedures
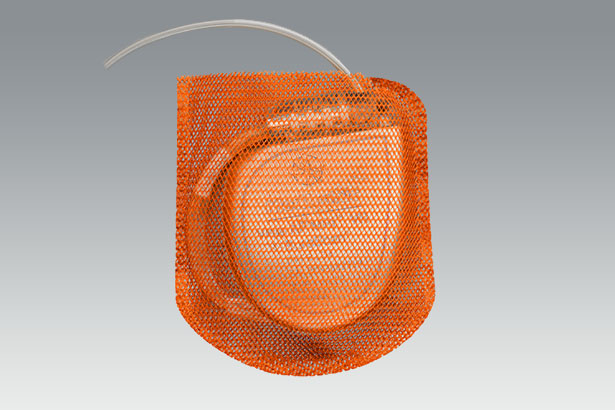
April 1, 2019 — Englewood Hospital recently took part in a landmark clinical trial. The trial assessed the capability of a novel, fully absorbable, single-use antibacterial envelope to reduce infections associated with the cardiac implantable electronic devices (CIEDs) it holds, and found positive results.
The World-wide Randomized Antibiotic Envelope Infection Prevention Trial (WRAP-IT) is the largest, randomized, global, prospective, multicenter, single-blinded, post-market, interventional trial ever conducted with CIEDs. It compared the incidence of major infections in patients whose CIED implantation included the TYRX envelope and patients whose procedure did not. Patients in the trial, sponsored by Medtronic, were followed for a minimum of 12 months.
Meeting its primary objective, WRAP-IT demonstrated that the Medtronic TYRX™ Absorbable Antibacterial Envelope reduced the risk of major infection by 40 percent, and pocket infection by 61 percent, in patients at increased risk for infections receiving CIEDs, compared to standard-of-care pre-operative antibiotic therapy. The average cost of a CIED infection in the United States ranges from $44,000–$83,000.
The trial also met its safety objective: the envelope did not increase the risk of procedure-related or system-related complications through 12 months. Englewood Hospital enrolled 38 patients between 2015 and 2017.
 “The reduced risk of infection is invaluable to patients undergoing CIED procedures,” said Grant Simons, MD, chief of heart rhythm services at Englewood Health. “Englewood Hospital’s participation in the trial helped generate strong clinical data showing that the use of the TYRX envelope can translate to shorter hospital stays and decreased necessity for post-operative antibiotic treatment.”
“The reduced risk of infection is invaluable to patients undergoing CIED procedures,” said Grant Simons, MD, chief of heart rhythm services at Englewood Health. “Englewood Hospital’s participation in the trial helped generate strong clinical data showing that the use of the TYRX envelope can translate to shorter hospital stays and decreased necessity for post-operative antibiotic treatment.”
Millions of people with life-threatening heart conditions opt for a CIED, such as a pacemaker, implantable cardioverter defibrillator (ICD) or cardiac resynchronization therapy (CRT) device, to help manage abnormal heart rhythms. Constructed from a multifilament, knitted absorbable mesh, the TYRX envelope is designed to stabilize these devices while releasing antimicrobial agents over a minimum of seven days, and is fully absorbed by the body approximately nine weeks after implantation.
As with any surgical procedure, there is risk for infection due to bacteria being introduced at the time of implant. Infections associated with these heart device implants are rare, occurring in 1–4 percent of all CIED patients and about 3 percent of high-risk patients. But the consequences can be devastating, including prolonged hospitalization, device removal and treatment with systemic antibiotics, and increased risk of dying.
Bacterial infection is one of the most common causes of CIED complications. While infection typically occurs in the first 90 days, bacteria introduced during the implant can lay dormant in the subcutaneous pocket that holds the device and can cause a delayed infection six months or more after implantation.
WRAP-IT was conducted in 181 centers in 25 countries in North America, Europe, Asia and South America, and included 776 implanting physicians. A total of 7,075 patients were enrolled from January 2015 through July 2017: 6,983 patients were randomized, with 3,495 receiving the TYRX envelope, and 3,488 randomized to the control group (without the envelope).
The trial results were recently presented in a late-breaking session at the American College of Cardiology‘s 68th Annual Scientific Sessions this month and published simultaneously in The New England Journal of Medicine.
The TYRX envelope was cleared by the FDA in 2013 and received CE Mark in 2014.
Englewood Hospital Receives National Reaccreditation in Bariatric Surgery
 March 27, 2019 — Patients seeking surgical treatment for severe obesity and related conditions have access to a nationally accredited program meeting the highest standards for patient safety and quality of care in the North Jersey area.
March 27, 2019 — Patients seeking surgical treatment for severe obesity and related conditions have access to a nationally accredited program meeting the highest standards for patient safety and quality of care in the North Jersey area.
 James McGinty, MD, chief of surgery at Englewood Health, specializing in laparoscopic bariatric surgery, recently announced its bariatric surgery program received reaccreditation as a distinguished three-year Comprehensive Center under the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP®), a joint program of the American College of Surgeons (ACS) and the American Society for Metabolic and Bariatric Surgery (ASMBS).
James McGinty, MD, chief of surgery at Englewood Health, specializing in laparoscopic bariatric surgery, recently announced its bariatric surgery program received reaccreditation as a distinguished three-year Comprehensive Center under the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP®), a joint program of the American College of Surgeons (ACS) and the American Society for Metabolic and Bariatric Surgery (ASMBS).
This reaccreditation reinforces Englewood Hospital’s commitment to providing and supporting quality improvement and patient safety efforts for metabolic and bariatric surgery patients. The MBSAQIP Standards ensure that bariatric surgical patients receive a multidisciplinary program—not just a surgical procedure—which improves patient outcomes and long-term success. The accredited center offers preoperative and postoperative care designed specifically for their severely obese patients.
Englewood Health’s commitment to quality care begins with appropriately trained staff and the leadership of surgeons who participate in meetings throughout the year to review its outcomes. They seek continuous improvement to enhance the structure, process, and outcomes of the center. Englewood Hospital was specifically recognized this year for its excellent leadership, strong hospital support, culture for doing bariatric surgery, and state-of-the-art facilities.
“I am proud to be a part of Englewood Health and this team of caregivers who really provide world-class care to patients suffering with obesity,” Dr. McGinty said. “This achievement is largely due to the leadership and support of the bariatric surgery team.”
To earn the MBSAQIP designation, Englewood Hospital met essential criteria for staffing, training, facility infrastructure, and protocols for care. The center also participates in a national data registry that yields semiannual reports on the quality of its processes and outcomes, identifying opportunities for continuous quality improvement.
After submitting an application, centers seeking MBSAQIP Accreditation undergo an extensive site visit by an experienced bariatric surgeon, who reviews the center’s structure, process, and clinical outcomes data. Centers are awarded a specific designation depending on how many patients they serve annually, the type of procedures they provide, and whether they provide care for patients under age 18.
In the United States, around 15.5 million people suffer from severe obesity, according to the National Institutes of Health, and the numbers continue to increase. Obesity increases the risks of morbidity and mortality because of the diseases and conditions commonly associated with it, such as type II diabetes, hypertension, and cardiovascular disease, among other health risks.
Metabolic and bariatric surgical procedures have proven to be effective in the reduction of comorbid conditions related to severe obesity. Working with ASMBS, the ACS expanded this quality program for bariatric surgery centers so that it can assist bariatric patients in identifying those centers that provide optimal surgical care.
Ask the Doctor: Dr. Samuel Bae
What are the most common symptoms that prompt patients to seek the help of a gastroenterologist?
Dr. Bae: I see many patients complain of heartburn and reflux. These symptoms are caused by a number of reasons, often poor diet and lifestyle. As you gain weight you become more likely to develop heartburn and reflux, which are major risk factors for esophageal cancer—so this is something to take seriously. I also see patients with bowel irregularities like diarrhea and constipation. If we can rule out major issues, these symptoms typically resolve with simple lifestyle changes. Many young men visit me saying they are bleeding during bowel movements. The culprit in this scenario is often spending too much time on the toilet with an electronic or mobile device. I tell them the recommended toilet time is 3-5 minutes.As a GI doctor, what conditions or diseases do you spend the most time treating?
Dr. Bae: I treat the standard gamut of GI ailments: reflux, irritable bowel syndrome and bowel irregularities. I completed my training at Memorial Sloan Kettering, so I also focus on cancer prevention. Chronic heartburn and reflux, also called gastroesophageal reflux disease (GERD), can lead to esophageal cancer—so instead of taking an antacid, those experiencing GERD should seek medical attention. Colon cancer is now the second leading cancer killer in the United States; it’s also one of the most treatable cancers. During a colonoscopy we are often able to remove the cancer-causing polyps and cure the patient right then and there. Unfortunately, in many cases, colon cancer does not cause any physical symptoms, which is why I always recommend a colonoscopy beginning at age 50 for those at average risk.Are colonoscopies as uncomfortable as they are made out to be?
Dr. Bae: Today’s colonoscopies are very different from those of the past. I remember when a colonoscopy meant days of liquid fasting, a gallon of preparation material and an enema as a chaser. Today, our prep material is much smaller, split over several days, and we only require a half day or so of fasting. With the sedation we use now, and the fact that the procedure is very quick, most patients can’t believe that the procedure was already performed when they wake up. Posted March 2019Englewood Health Among First in Region to Implant 100th WATCHMAN Device
March 13, 2019 – Englewood Health is among the first hospitals in North Jersey to complete its 100th implant of the lifesaving WATCHMAN device, which reduces the risk of blood clots, stroke, and death in patients with irregular heartbeat without long-term blood-thinning medications.
For patients on blood thinners—which is most patients with atrial fibrillation—something as simple as a fall or as major as a car accident could cause harmful, even fatal, internal bleeding. The WATCHMAN device allows patients to stop taking these medications and return to active lifestyles with less fear and fewer changes.
 “Patients who can’t tolerate blood thinners are really in a tough situation because they need blood thinners to prevent stroke, but if they take blood thinners they have bleeding complications,” said Grant Simons, MD, chief of heart rhythm services at Englewood Health. “For those with non-valvular atrial fibrillation who are seeking an alternative to warfarin, the WATCHMAN implant offers a potentially life-changing stroke-risk treatment option, which could free them from the challenges of long-term warfarin therapy.”
“Patients who can’t tolerate blood thinners are really in a tough situation because they need blood thinners to prevent stroke, but if they take blood thinners they have bleeding complications,” said Grant Simons, MD, chief of heart rhythm services at Englewood Health. “For those with non-valvular atrial fibrillation who are seeking an alternative to warfarin, the WATCHMAN implant offers a potentially life-changing stroke-risk treatment option, which could free them from the challenges of long-term warfarin therapy.”
In a clinical trial, nine out of 10 people were able to stop taking warfarin in 45 days after the WATCHMAN procedure.
The size of a quarter, the WATCHMAN device fits into the left atrial appendage (LAA), where 90% of stroke-causing blood clots that originate in the heart are formed. The implant permanently closes off this part of the heart to keep those blood clots from escaping, entering the blood stream, and traveling to the brain, lungs, and other parts of the body.
The WATCHMAN implant, performed via a catheter inserted in the groin, is a one-time procedure that lasts about an hour, followed by an overnight hospital stay with most patients leaving the next day.
Candidates for the device include patients who have atrial fibrillation not caused by heart valve problems, are able to take short-term blood-thinning medications after the procedure, and are poor candidates for long-term blood-thinning medications.
Atrial fibrillation is a common condition affecting more than five million people in the United States. It causes blood to pool in the LAA, sometimes leading to the formation of clots that can break loose and travel up to the brain, potentially causing a stroke. In fact, people with atrial fibrillation have five times the risk of stroke than compared to those with a regular heartbeat.
The WATCHMAN device has been implanted in more than 10,000 patients and is approved in more than 70 countries around the world. Manufactured by Boston Scientific Corporation, the WATCHMAN implant was approved by the Food and Drug Administration in 2015. Englewood Health had performed northern New Jersey’s first implant during the second phase of its national clinical trial back in 2012. Englewood Health’s 100th WATCHMAN procedure came at the close of American Heart month this year.
“We continue to be at the forefront of available technologies,” said Dr. Simons. “This is a relatively new procedure that we were able to introduce to the medical community and deliver to our patients through a high-volume, high-quality program developed safely in a short amount of time.”
Ask the Doctor: Dr. Anna Serur
What’s the difference between Crohn’s disease, ulcerative colitis, and diverticulitis?
Dr. Serur: Crohn’s disease is an inflammatory disease that can affect anywhere in the intestinal tract, from end to end. Crohn’s patients have periods of active disease, or flare-ups, when they experience signs and symptoms, and periods of remission, when the signs and symptoms cease. Ulcerative colitis is an inflammatory disease that causes long-term inflammation and ulcers (sores) contained to the lining of the colon. Signs and symptoms develop over time, rather than suddenly. Diverticulitis is an inflammation or infection of small pouches that form along the intestinal wall. These pouches most commonly develop in the sigmoid colon and can cause acute or chronic signs and symptoms.What signs and symptoms should I watch for?
Dr. Serur: For Crohn’s disease and ulcerative colitis, symptoms can include intense abdominal pain, severe chronic diarrhea, weight loss, malnutrition, and fatigue. Both conditions can be very debilitating and lead to life-threatening complications such as severe bleeding, perforation of the colon, severe dehydration, and rapid swelling of the colon. The most common signs and symptoms of diverticulitis are severe abdominal pain and fever.How are these diseases treated?
Dr. Serur: There are many successful, well-tolerated medications used to treat Crohn’s disease and ulcerative colitis. In cases where medical treatment and lifestyle modifications are not effective enough at controlling the disease, surgery may be necessary. Over the past 10 years, diverticulitis treatment protocols have evolved. Surgery is recommended for some patients experiencing attacks or complications. The good news is we know a lot more about these diseases today than we did even five years ago. As a result, treatments are becoming more individualized.Is there anything I can do to prevent these illnesses?
Dr. Serur: Unfortunately there is no way to prevent Crohn’s disease or ulcerative colitis. But better nutrition, lifestyle changes, and smoking cessation for those who smoke can help alleviate symptoms. Eating a high-fiber diet, drinking plenty of fluids, and getting sufficient exercise may help to prevent diverticulitis. Because stress can bring on flare-ups of all three conditions, it is vital that patients develop a stress management routine. Exercise is particularly helpful—go to the gym, do Pilates or yoga. While these conditions are complex, they are compatible with a normal lifestyle. Under a physician’s care, patients should not be afraid to go on with their lives. Posted March 2019Palliative Medicine and Hospice Specialist Vinnidhy Dave, DO, Appointed Director of Palliative Medicine at Englewood Health Physician Network
March 11, 2019 – Palliative medicine and hospice specialist Vinnidhy Dave, DO, has been appointed director of palliative medicine at Englewood Health Physician Network. Dr. Dave joins Englewood Health from the Hospital for Special Surgery in New York, where he was director of medical pain management and a clinical instructor at Weill Cornell Medical College. He completed both clinical and research fellowships in hospice and palliative medicine at Memorial Sloan Kettering Cancer Center.
Dr. Dave’s particular clinical interests include cancer pain management, pain management in patients with multiple medical conditions not eligible for interventional treatment, symptom management for oncology patients, and advanced care planning.
“As a palliative medicine specialist, I focus on individualizing care for my patients to improve their symptoms and quality of life while they undergo treatment for their disease,” says Dr. Dave. “With my cancer patients, I focus on helping them to manage pain, nausea, loss of appetite, and other often disabling symptoms. I view each patient as a human being, not as a diagnosis; I believe this is important for the patient–physician relationship and leads to the best clinical results.”
“I am honored to join the Englewood Health Physician Network,” he adds, “where I will collaborate with oncologists and other specialists throughout the network, to provide coordinated care for our patients through close communication and a shared electronic medical record.”
Dr. Dave is board certified in hospice and palliative medicine and in internal medicine. He received his DO from New York College of Osteopathic Medicine and did his internal medicine residency at the University of Medicine and Dentistry of New Jersey.
“We are very excited to welcome Dr. Dave to our team of renowned specialists and providers. Dr. Dave’s expertise in palliative medicine will help meet an important need in our community,” said Dr. Stephen Brunnquell, president of the Englewood Health Physician Network. “As our network continues to grow, we remain focused on ensuring that our patients have access to leading care right here, in their own backyard.”
A member of the American Academy of Hospice and Palliative Medicine and the American Pain Society, Dr. Dave is the co-author of several scientific publications on pain management and palliative care and has presented his research at national medical society meetings.
Englewood Hospital Named One of America’s 50 Best for Vascular Surgery
February 20, 2019 – Englewood Hospital is the only New Jersey hospital to be named one of America’s 50 Best Hospitals for vascular surgery by Healthgrades® and receive the Healthgrades 2019 Vascular Surgery Excellence AwardTM.
The achievements are part of findings released in the Healthgrades 2019 Report to the Nation. The new report demonstrates how clinical performance differs dramatically among hospitals nationally, regionally and locally, and the impact that this variation has on health outcomes.
During the 2015-2017 study period, Healthgrades found that:
- Patients treated at hospitals receiving the America’s 50 Best Hospitals for Vascular Surgery award have, on average, a 40 percent lower risk of experiencing a complication while in the hospital than if they were treated in hospitals that did not receive the award
- Patients treated at hospitals which did not receive the America’s 50 Best Hospitals for Vascular Surgery were, on average, 1.67 times more likely to experience one or more complications in the hospital than if they were treated at hospitals that did receive the award*
“Being named one of America’s 50 Best Hospitals for vascular surgery is a strong testament to our long history as a leader in vascular surgery and our ongoing efforts to bring the safest, highest-quality, and most technologically advanced care to our community,” said Warren Geller, president and CEO of Englewood Health. “We thank our doctors, nurses, and other staff for their tireless efforts to make us who we are and congratulate them on this recognition of excellence by Healthgrades.”
Englewood Health has established itself as a leading center for vascular and endovascular treatment through surgical and non-surgical techniques, state-of-the-art diagnostics, and an ongoing commitment to patient care, research, and training. Most recently, Englewood became one of the first hospitals in New Jersey to offer a new, minimally invasive procedure to treat severe carotid artery disease. The procedure, called transcarotid artery revascularization (TCAR), is unique in that blood flow is temporarily reversed during the procedure so that any small bits of plaque that may break off in the artery are diverted away from the brain, which helps prevent a stroke. A stent is then placed inside the artery to stabilize the plaque, minimizing the risk of a future stroke.
“Hospitals that have achieved the Healthgrades America’s 50 Best Hospitals for vascular surgery have proven their dedication to quality care and exceptional outcomes,” said Brad Bowman, MD, chief medical officer at Healthgrades. “Consumers should consider hospital quality when navigating their care journeys, and this recognition distinguishes Englewood Hospital in the marketplace.”
Englewood Hospital was also recognized for the following clinical achievements:
- Five-star recipient for hip fracture treatment in 2019
- Five-star recipient for carotid surgery in 2019
- Five-star recipient for gallbladder removal surgery in 2019
- Five-star recipient for appendectomy for 3 years in a row (2017-2019)
* Statistics are based on Healthgrades analysis of MedPAR data for years 2015 through 2017 and represent 3-year estimates for Medicare patients only.
Englewood Health Recognizes American Heart Month
February 15, 2019 — In recognition of American Heart Month Englewood Health is participating in the American Heart Association’s Little Hats Big Hearts program to send more healthy babies and moms home by raising awareness and advocating for change.
Throughout the month of February, new moms at Englewood Hospital are beginning their parenthood journeys with support and information including tips on raising a healthy family, at-home exercise ideas, and heart-healthy recipes. Their babies are receiving red caps, handmade by volunteers from across New Jersey, for safeguarding through the cold winter months.
Each year in the United States 36,000 children are born with a heart defect, increasing their risk of developing medical conditions such as pulmonary hypertension, infective endocarditis, congestive heart failure, anticoagulation, and arrhythmias. With the right care, however, most defects are possible to fix. Englewood Health is proud to play a part in helping new parents better care for themselves and their newborns.
The New Jersey Little Hats Big Hearts initiative is sponsored locally by Novartis.