When the Department of Cardiothoracic Surgery at Englewood Hospital and Medical Center was founded in 2000, James Klein, MD, chief, cardiothoracic surgery, made a commitment to create a culture of caring and cooperation. To accomplish this, the department initiated a new policy: Two surgeons would be required to oversee each surgery in the operating room. The thinking behind this policy was to have a built-in safety net during every procedure.

“Our goal was to foster a teamwork environment,” Dr. Klein said. “We followed a mantra of cohesiveness and helping each other, not a mantra of competition. We were striving for perfection in terms of outcomes.”
The efforts of the cardiothoracic team have paid off. Over the last 17 years, the department has performed close to 4,800 heart operations.
The hospital’s mortality and survival data for bypass surgery also show the department’s success in building a durable safety net. The overall survival rate for isolated bypass surgery since the inception of the cardiothoracic program is approximately 99%.
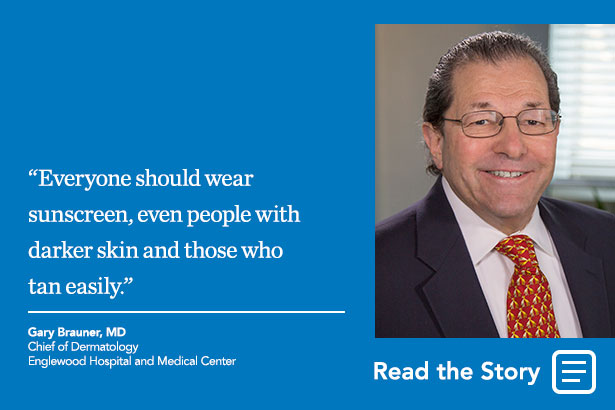
Many factors contribute to this low mortality rate. One is the department’s careful blood transfusion policy.
“Blood transfusions can lead to inflammatory and immune response reactions,” Dr. Klein explained. “If you can avoid both, you’re probably ahead of the game because you’ve succeeded in eliminating one set of complications and compounding issues.”
The cardiothoracic team pays closer attention to what’s happening to the patients’ organs than to their blood counts. They have taken the position that if the brain, heart, lungs, and kidneys are functioning properly, they will forgo a blood transfusion—even if a patient’s blood count is low.
“The Society of Thoracic Surgeons (STS) has established guidelines similar to what we’ve been doing for years,” Dr. Klein said. “We were among the first institutions to follow this practice.”
Since 2012, the department has ventured into a new arena: performing transcatheter aortic valve replacement (TAVR), also known as transcatheter aortic valve implantation. The procedure is performed by cardiothoracic surgeons in partnership with interventional cardiologists. TAVR is typically performed in Englewood Hospital’s new, state-of-the-art hybrid operating room.
Prior to the introduction of TAVR, the only option was for surgeons to go through the chest to replace the aortic valve, but that approach is being used less frequently. Instead, surgeons are inserting the new valve up through the femoral artery in the groin. The old valve is left in place and simply pushed aside. TAVR is performed on patients suffering from aortic stenosis, or a narrowing of the aortic valve. The Department of Cardiothoracic Surgery has performed more than 250 TAVR procedures, with numbers increasing each year.
Originally, TAVR was confined to older or frailer patients, but that is changing, according to Dr. Klein. An increasing group of intermediate-risk patients, who are younger and less frail, are now opting for TAVR. As the number of patients documented in New Jersey and STS databases grows, Englewood Hospital can use this information to compare its morbidity and mortality data with other institutions in the state and region.
“Although there is the potential for leg complications, doing the whole operation without touching the chest is less invasive and less aggressive,” Dr. Klein said. “The procedure can be done in about an hour and often results in shorter stays in the hospital and an easier recovery for the patient.”
These innovations have not gone unnoticed. Over the last two years, the department has experienced tremendous growth and expanded significantly, with 2017 likely to be the busiest year yet.
“Our efforts in blood conservation and TAVR have put us on the map. As a result, we have growing local, regional, and national reputations,” Dr. Klein said.
Posted September 2017