latest screenings and treatments for lung and GI cancers in Asian populations.
Physicians and other health care professionals gathered at an education seminar at Englewood Hospital and Medical Center to discuss the prevalence of lung and gastrointestinal cancers in Asian populations and some of the medical center’s personalized treatments.
The Lefcourt Family Cancer Treatment and Wellness Center at Englewood Hospital hosted its second annual cancer symposium to review the latest screenings and treatments for lung and GI cancers in high-risk populations, particularly in the Asian and Asian American populations, who are at greater risk for developing certain cancers, such as liver and stomach cancer.
“We’re honored to take care of specialized populations in this cancer center, and we want to bring to the forefront screening identification, prevention and treatment for patients who are living with or surviving these types of cancers,” said Steven Brower, MD, medical director of the cancer center and chief of surgical oncology and hepatobiliary surgery at Englewood Hospital.
Dr. Brower spoke about identifying GI cancers early and determining the differences between Asian Americans and those from other ethnicities who develop the malignancy.
According to the National Cancer Institute, liver and stomach cancer incidence and mortality are highest among Asian Americans compared with all other ethnic groups. A 2016 report from the American Cancer Society estimates there will be 57,740 new cancer cases and 16,910 cancer deaths among Asian Americans, Native Hawaiians and Pacific Islanders annually. There is a need for improved use of vaccinations and screenings, interventions to control weight, alcohol and tobacco use, and more research on the differences in cancer burdens in this population.
“Here in Bergen County, we have a very high population of Asians, especially Koreans, and recognizing a need to understand the specific risks that this patient population has and how to best treat them is the focus of our talks,” said Brian Kim, MD, a hematology/oncology specialist at Englewood Hospital, and the moderator of the symposium.
Advances in Lung Cancer Screening
Englewood Hospital’s radiology department is currently working with primary care physicians, internists and family practitioners to identify patients at risk for lung cancer and initiate screening earlier.
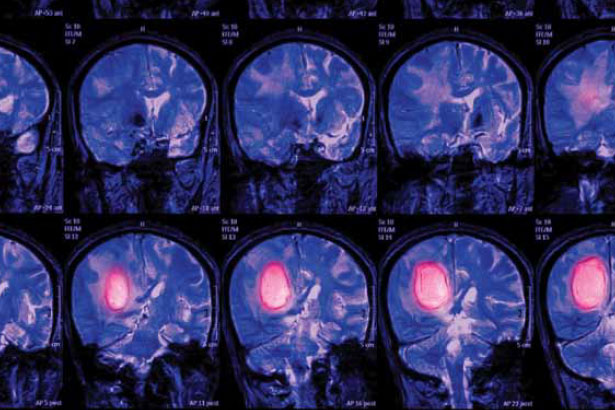
Mark Shapiro, MD, chief of radiology at Englewood Hospital, spoke at the cancer symposium about the role of low-dose CT scans for screening patients for lung cancer. He said patients must meet the criteria for screening guidelines (age range, 55-77 years with a strong smoking history) in order to undergo CT.
“CT has been proven in various studies to decrease the mortality from lung cancer. It’s critical that when clinicians see patients that fall into the guidelines for the screening that they undergo this low-dose screening CT scan,” Dr. Shapiro said.
Lyall Gorenstein, MD, a thoracic surgeon at Englewood Hospital, presented ways to use thoracic surgery and minimally invasive techniques to diagnose and manage solitary pulmonary nodules and avoid unnecessary lung biopsies.
“That’s a key goal of any multidisciplinary team, to really expedite the care rather than have patients being shuffled between one doctor and another, so time goes on and their anxiety about their cancer builds,” Dr. Gorenstein said. “Being able to offer one-stop shopping in a very beautiful environment – that’s something I think makes Englewood a little unique compared to our regional competitors.”
The oncology team at Englewood Hospital is committed to working with other departments and outside health care providers to treat high-risk populations who have cancer, and offer screening and preventive services to patients as soon as they are identified to be at risk.
“Our physicians in the cancer center are at the forefront of identification of high-risk patients, and those of us who actually treat the patients hope to get these patients early,” Dr. Brower said.
Posted March 2017